Sales of prescription opioids in the U.S. nearly quadrupled from 1999 to 2014, with more than half prescribed to adults with mental health disorders.
Adults living with depression, anxiety and mood disorders receive 51 percent of all opioid prescriptions, despite representing only 16 percent of the nation’s overall population. To combat the growing national opioid epidemic, it is critical that we begin to rethink pain management among this group. (“Study Links Mental Health Disorders with Greater Use,” The Tennessean, July 9, 2017.)
Chronic pain is an ongoing problem for many people with depression and anxiety; it is also a common risk factor for suicide. Over the last decade, chronic pain has been largely responsible for the spike in opioid prescriptions.
The key to solving this widespread issue is clear to Brian Sites, an anesthesiologist at the Dartmouth-Hitchcock Medical Center who co-authored a study published in the Journal of the American Board of Family Medicine on prescription medications among people with mental illness.
“This isn’t a drug cartel problem,” Sites said. “This is a physician prescribing problem. We know where it starts.”
To target the root of the problem, more tools and trainings must be made available.
Tennessee, which leads the nation in the number of opioid prescriptions per person, is supplementing mandatory training for medical professionals with education for both doctors and patients to help them manage “complex medical conditions while managing pain with alternative treatment models.”
Centerstone, a behavioral health center that treats more than 65,000 people in Tennessee, recently launched an anxiety recovery program aimed at educating patients with chronic anxiety about how their condition interacts with physical pain. The Tennessee Department of Mental Health and Substance Abuse Services also launched an initiative to create a protocol for emergency rooms to identify people with anxiety or depression and treat them for those conditions without prescribing opioids.
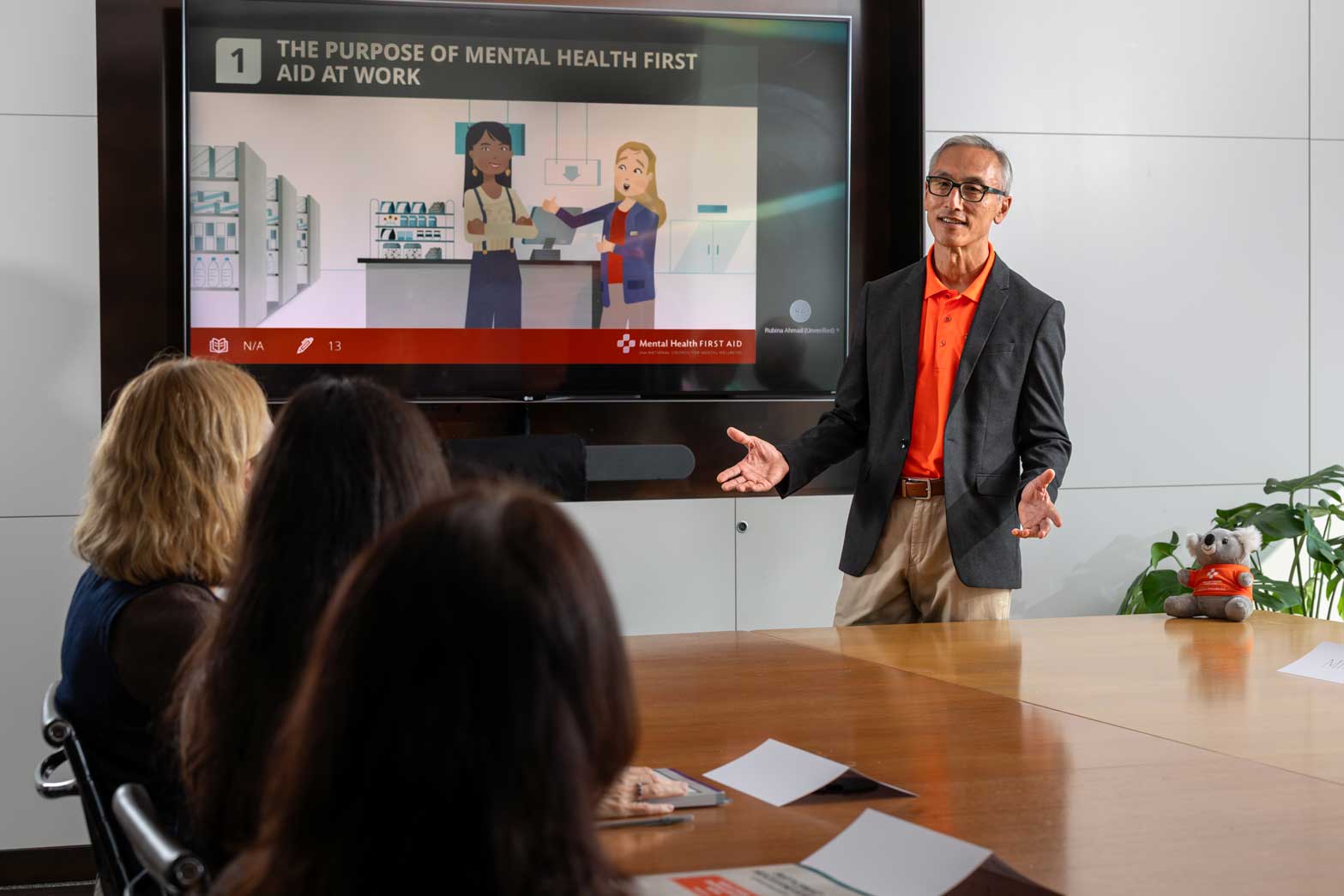
Trainings and initiatives like these help patients manage their mental health challenges, as well as their pain, with alternative treatment models. To divert people from prescribing and using opioids, we must first understand the connection between mental health and substance use disorders. Mental Health First Aid bridges that gap. It is a course that offers information on both mental health and substance use, and provides the whole picture about their complex relationship.
Take a Mental Health First Aid course today.
To learn more about alternative treatment models for chronic pain management, check out our BH365 Blog, Finding the Right Alternative for You: Managing Chronic Pain.